Looking for ways to calm an IBS flare up? You're not alone. Irritable bowel syndrome (IBS) is a common gastrointestinal condition affecting around 15% of people, with symptoms including stomach cramps, bloating, diarrhea, and constipation. Although IBS is typically a chronic (long-lasting) condition, many people's symptoms come and go. If you're experiencing an increase in symptoms, here are some helpful strategies to soothe an IBS flare-up.
What is an IBS flare-up?
An IBS flare-up (sometimes called an IBS attack) is a period when your usual gut symptoms suddenly become more intense or unpredictable. You might feel stronger stomach cramps, bloating, or changes in bowel habits — like constipation, diarrhea, or both. For some people, a flare-up can last a few hours and then ease on its own. For others, it can stretch out for days or even weeks, making everyday life feel uncomfortable and unpredictable.
IBS flare-ups can happen for many reasons, including stress, certain foods, hormonal changes, or even a simple shift in routine. But sometimes, they seem to appear without any clear trigger — even when you’re doing all the “right” things. While IBS can’t be cured, understanding how flare-ups work is the first step to managing them and finding ways to calm your gut when symptoms strike.
What is the difference between an IBS flare-up and an IBS attack?
The terms IBS flare-up and IBS attack are often used interchangeably, but they can describe slightly different experiences. Both refer to times when IBS symptoms suddenly worsen, leading to pain, bloating, and changes in bowel habits.
Generally, a flare-up describes a short-term increase in symptoms that may be triggered by stress, certain foods, hormones, or routine changes. An attack, on the other hand, usually refers to a more intense and prolonged episode that can last for days or even weeks. IBS attacks may involve stronger pain, more frequent bathroom trips, and greater disruption to daily life.
While there’s no medical distinction between the two, many people use IBS attack to describe the more severe end of the IBS spectrum – when symptoms feel overwhelming or unmanageable and may require extra care or professional support.
What causes an IBS flare-up or IBS attack?
The exact cause of IBS flare-ups isn’t fully understood, but research shows several factors can trigger or worsen symptoms. These triggers can vary widely from person to person – what causes a flare-up for one individual may not affect another.
Common IBS flare-up and attack triggers include:
• Eating ‘trigger’ foods: High-FODMAP foods – such as onions, garlic, beans, wheat, and some fruits – can be difficult for the gut to digest and may increase gas, bloating, and abdominal discomfort.
• Stress: Both short-term and chronic stress can intensify gut sensitivity and change how the intestines move. Emotional stress from work, relationships, or major life changes often plays a key role in IBS symptom flare-ups.
• Gastrointestinal infections: A gut infection, like gastroenteritis or food poisoning, can sometimes lead to post-infectious IBS or trigger ongoing digestive sensitivity.
• Psychological factors: Anxiety, depression, and post-traumatic stress can heighten communication between the brain and gut, increasing symptom severity and frequency.
Understanding your unique triggers is an important step toward preventing future flare-ups and managing IBS more confidently.
What does an IBS flare-up or attack feel like?
An IBS flare-up can feel different for everyone. Some people experience symptoms almost every day, while others go weeks or even months without any issues. When a flare-up happens, it usually means your IBS symptoms have suddenly intensified and are lasting longer than usual.
Common symptoms of an IBS flare-up or attack include:
• Abdominal pain or cramping (a hallmark IBS symptom)
• Bloating or visible swelling in the abdomen
• Excessive gas or burping
• A sensation of incomplete bowel emptying after passing stool
• Diarrhea, constipation, or alternating between both
Other symptoms some people notice during an IBS flare-up include:
• Headaches or body aches
• Joint or muscle pain
• Fatigue or low energy levels
• More frequent urination
• Heightened feelings of anxiety, stress, or low mood
These symptoms can vary in intensity from day to day – and sometimes from hour to hour – making IBS flare-ups unpredictable and difficult to manage.

How long does an IBS flare-up last?
The duration of an IBS flare-up can vary widely from person to person. For many, symptoms peak over two to four days before easing, but others may find that flare-ups linger for a week or more. Some people experience IBS in waves – where symptoms come and go over several days or even weeks.
How long a flare-up lasts often depends on your triggers, stress levels, and how quickly you can calm your gut once symptoms begin. The good news is that with the right management techniques – such as relaxation, dietary adjustments, and mind-body therapies – you can often reduce the intensity or shorten the duration of an IBS flare-up.
What to eat during an IBS flare-up or IBS attack
It can be hard to know what to eat when you’re in the middle of an IBS flare-up. Foods that are high in FODMAPs – small carbohydrate molecules that feed gut bacteria and produce gas – are among the most common triggers. Research shows that following a low FODMAP diet can significantly reduce IBS symptoms for many people.
To help calm an IBS flare-up, try avoiding high FODMAP foods such as:
• Fructans – found in garlic, onion, wheat, rye, and broccoli
• Oligosaccharides – found in chickpeas, lentils, beans, and some forms of tofu
• Lactose and dairy products – including cow’s milk, yogurt, and ice cream
• Fructose (fruit sugar) – found in apples, mangoes, watermelon, and honey
• Polyols (sugar alcohols) – found in nectarines, peaches, plums, cauliflower, and mushrooms
Instead, choose gentle, low-FODMAP foods such as:
• Grains – gluten-free oats, white rice, brown rice, and basmati rice
• White meats – poultry and fish
• Cooked vegetables – carrots, potatoes, peas, Swiss chard, eggplant, and kale
• Nuts and seeds – flaxseed, pecans, pine nuts, and small portions of almonds
A low FODMAP diet is typically followed in two stages – first by eliminating high FODMAP foods for several weeks, then slowly reintroducing them one at a time while tracking symptoms. This approach can help identify which foods trigger your IBS flare-ups and which your gut tolerates best.


Calm your IBS in 6 weeks
Take our free assessment to discover if Nerva can work for you.
✅ 89% success rate
✅ 80,000+ people helped
✅ Created by gut health experts
❌ No appointments or waitlists
❌ No pills or diet change
Start assessmentHot Flash Relief
Manage your hot flashes in just 5 weeks.
✅ Science-backed & effective
✅ Natural & safe option
✅ Created by Dr Elkins
❌ No appointments or waitlists
❌ No medications
Learn moreRefer, monitor and grow
A free and easy way to refer patients to digital hypnotherapy programs.
Let's Connect.webp)
.webp)
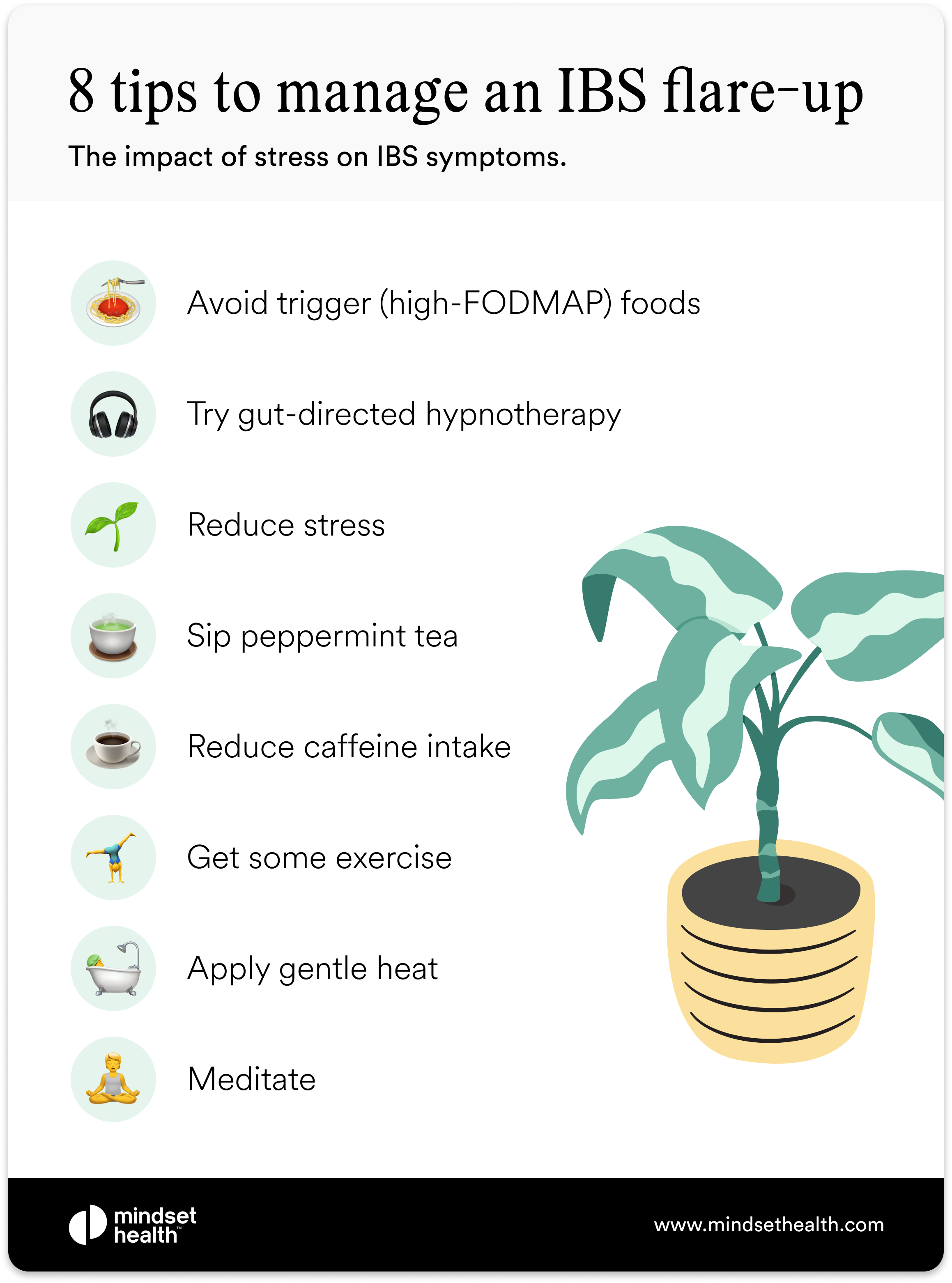
What are some effective strategies to calm an IBS flare-up?
When IBS symptoms flare up, small changes to your routine can help calm your gut and shorten the duration of discomfort. Here are some of the most effective, evidence-based ways to manage an IBS flare-up or attack:
1. Try gut-directed hypnotherapy
Gut-directed hypnotherapy is a natural, evidence-based way to reduce IBS symptoms without medication or restrictive diets. It involves entering a relaxed, focused state and using visualization to retrain the gut-brain connection.
Clinical studies show gut-directed hypnotherapy can be just as effective as the low FODMAP diet, with more than half of participants reporting significant symptom relief. You can access this therapy through a certified hypnotherapist or via digital programs such as the Nerva app, which is based on clinical research.
Hypnotherapy can help by:
• Reducing pain sensitivity in the brain
• Restoring healthy gut-brain signaling
• Lowering anxiety and stress that can worsen gut discomfort
2. Reduce stress
Because the gut and brain are directly connected, emotional stress often leads to digestive stress. Calming the mind helps regulate the gut and ease symptoms.
Two proven methods include:
• Mindfulness meditation – Studies show meditation can reduce bloating, cramping, and pain by calming the body’s stress response.
• Yoga – A combination of movement and breathwork that supports both digestive function and emotional regulation.
3. Try peppermint oil
Peppermint oil has long been used as a natural digestive remedy and is approved by the FDA for IBS treatment. Its active compound, menthol, relaxes the muscles of the colon and soothes pain receptors.
Peppermint oil capsules can help reduce pain, bloating, and constipation and have been shown in studies to be more effective than some antispasmodic drugs. If you’re sensitive to supplements, sipping peppermint tea offers a gentler alternative.
4. Reduce caffeine intake
Caffeine can stimulate the intestines and worsen diarrhea or urgency. During a flare-up, try eliminating caffeine completely – including coffee, black and green tea, energy drinks, soft drinks, and chocolate – to see if symptoms improve.
5. Apply gentle heat
Heat therapy can relax the abdominal muscles and ease cramping. Place a warm heat pack or hot water bottle over your stomach for 15–20 minutes (with a towel to protect your skin). Many people find this simple approach offers quick, soothing relief.
6. Get some exercise
Light movement helps your gut regain rhythm and reduces stress hormones that fuel flare-ups. Even a short walk, gentle yoga flow, or low-impact workout can improve bloating and abdominal pain. Regular activity also supports better long-term symptom control.
Common medical treatments for IBS
Because the exact cause of IBS isn’t fully understood, treatment focuses on reducing symptoms and improving quality of life. For many people, diet and lifestyle changes are enough to bring relief. But if your symptoms persist, your healthcare provider may recommend one or more medical treatments.
Common IBS medications include:
• IBS-specific medications – Some drugs target IBS symptoms directly by slowing bowel movement to ease diarrhea or increasing fluid in the intestines to relieve constipation. Examples include alosetron (Lotronex) and lubiprostone (Amitiza).
• Antispasmodics – These relax the muscles of the colon to ease cramping and spasms. Hyoscine (Levsin) and dicyclomine (Bentyl) are common examples, though they can cause side effects such as dry mouth or dizziness.
• Antidiarrheals – Medications like loperamide (Imodium) can help control severe diarrhea. They should be used under medical guidance, as side effects may include nausea or stomach upset.
• Antidepressants – Low-dose antidepressants can help manage abdominal pain and regulate bowel movements. Options include tricyclic antidepressants such as imipramine (Tofranil) or SSRIs like citalopram (Celexa). These should always be prescribed and monitored by a doctor due to potential side effects.
When to see a doctor for IBS
If your IBS symptoms don’t improve with at-home care, or if you notice any of the following red flags, contact your healthcare provider as soon as possible:
• Persistent or worsening abdominal pain
• Blood in your stool or dark, tar-like stools
• Unexplained weight loss or ongoing fatigue
• Symptoms that wake you during the night
• Dizziness, lightheadedness, or fainting
• Loss of appetite, nausea, or vomiting
If you experience any of these symptoms, you should visit a doctor as soon as possible. In addition to assessing your symptoms, several tests can be performed to find out if you have a different medical condition.

FAQs about IBS flare-ups
1. How long does an IBS flare-up usually last?
IBS flare-ups can last anywhere from a few hours to several days, though some people experience symptoms that come and go over a few weeks. How long a flare-up lasts often depends on triggers, stress levels, and how quickly you can calm your gut.
2. What triggers an IBS flare-up?
Common IBS triggers include stress, hormonal changes, certain high-FODMAP foods, caffeine, and gastrointestinal infections. However, flare-ups can also occur without a clear cause.
3. How can I calm an IBS flare-up quickly?
You can try applying a heat pack, practicing relaxation techniques, taking a short walk, or using peppermint oil capsules. Some people also find gut-directed hypnotherapy helpful for reducing flare-up severity and preventing future episodes.
4. What foods are best during an IBS flare-up?
Gentle, low-FODMAP foods such as white rice, cooked carrots, potatoes, and lean proteins like chicken or fish are usually well tolerated. Avoid high-FODMAP foods like onions, beans, apples, and dairy until symptoms ease.
5. When should I see a doctor for IBS?
See a healthcare provider if you have blood in your stool, severe or persistent pain, vomiting, unexplained weight loss, or symptoms that wake you at night. These could indicate another digestive condition that needs medical attention.
The Wrap Up
An IBS flare-up can be frustrating and unpredictable, but there are proven ways to regain control. Simple at-home strategies such as gut-directed hypnotherapy, following a low-FODMAP diet, applying gentle heat, reducing caffeine, staying active, and managing stress can all help calm symptoms and support your gut-brain connection.
If flare-ups become frequent or your symptoms are hard to manage, speak with your healthcare provider. They can help rule out other digestive conditions and discuss medical treatments that may ease your discomfort. With the right combination of lifestyle changes, mind-body support, and professional care, most people find their IBS symptoms become milder and more manageable over time.
An IBS flare-up can be frustrating and may cause a range of digestive symptoms. If you’re experiencing a flare, there are several at-home remedies you can try, such as gut-directed hypnotherapy, removing high-FODMAP foods from your diet, heat therapy, avoiding caffeine, exercising, and reducing stress. You may also wish to talk to your healthcare provider about medications to treat IBS symptoms and check that another condition isn’t causing your digestive symptoms.
Want to calm your IBS in 15 minutes a day?
Take our free quiz to discover if Nerva's gut-directed hypnotherapy program can work for you.
✅ 89% success rate
✅ 80,000+ people helped
✅ Created by gut health experts
❌ No appointments or waitlists
❌ No pills or diet change
Start quizHot Flash Relief
Manage your hot flashes in just 5 weeks.
✅ Science-backed & effective
✅ Natural & safe option
✅ Created by Dr Elkins
❌ No appointments or waitlists
❌ No medications
Learn moreRefer, monitor and grow
A free and easy way to refer patients to digital hypnotherapy programs.
Let's ConnectTake the Quiz.
Take the Quiz.


.svg)

.png)







