We all know IBS can be a pain in the gut – but it can also cause discomfort in the back, head, and jaw. After bloating, pain is the most common IBS symptom, affecting more than 75% of people who experience frequent or constant abdominal discomfort. IBS pain is most often felt in the lower abdomen, but it can also appear in other areas of the body that are directly or indirectly connected through the gut-brain axis.
Understanding IBS pain: causes, locations, and relief strategies
IBS pain is one of the most common and distressing symptoms people experience – and it’s the number one reason people seek medical help for the condition. Read on to learn where IBS pain typically occurs, why it happens, and what you can do to find relief at home.
What is IBS pain?
IBS pain arises from miscommunication along the gut–brain axis – the two-way signaling system between your digestive tract and nervous system. This disrupted communication can heighten sensitivity in the intestines, making normal sensations feel painful or uncomfortable.
While IBS pain can appear in multiple areas of the body, it most often occurs in the lower abdomen, the region between the chest and pelvis. The discomfort may develop after eating and can sometimes improve – or worsen – after a bowel movement. The pain can range from a dull ache or cramp to sharp, stabbing sensations that are occasionally mistaken for appendicitis or even heart pain.
Common locations of IBS pain
People with IBS most often describe their pain in these areas:
- Lower abdomen: cramping, bloating, or fullness that may shift sides or radiate to the pelvis
- Upper abdomen or stomach area: pressure or burning sensations that worsen after meals
- Back or lower back: referred pain from intestinal muscle contractions or bloating
- Sides of the abdomen (flanks): discomfort linked to trapped gas or intestinal movement
Although abdominal pain is the hallmark of IBS, research shows that many people also experience headaches, back pain, and muscle aches, showing how the gut–brain connection influences the wider nervous system.
Diagnostic criteria for IBS pain
According to the Rome IV criteria – the current medical guidelines used to diagnose IBS – a person must experience:
- Recurrent abdominal pain, on average, at least one day per week in the last three months, and
- Pain associated with two or more of the following:
- Changes in bowel movements (either frequency or consistency)
- Pain related to defecation
- Altered stool form or appearance
If pain persists for more than six months, it’s considered chronic IBS pain. Chronic pain can mean ongoing discomfort most days or recurring pain episodes that last for long stretches of time.
Why IBS pain happens
IBS pain is thought to stem from increased visceral hypersensitivity – a heightened sensitivity of the intestinal nerves that amplifies pain signals sent to the brain. This sensitivity is often influenced by stress, gut inflammation, diet, and changes in the gut microbiome. For some, even mild gas or normal digestion can trigger severe discomfort due to this oversensitivity.
Managing IBS pain at home
While IBS pain can be intense and unpredictable, several at-home remedies can help:
- Heat therapy: applying a warm compress or heat pack can relax intestinal muscles and reduce cramping
- Gentle movement: low-impact activities like yoga or walking improve digestion and relieve tension
- Stress reduction: mindfulness, gut-directed hypnotherapy, and diaphragmatic breathing calm the vagus nerve and ease pain
- Dietary adjustments: tracking trigger foods or following a low-FODMAP plan under guidance can reduce flare-ups
- Regular meals and hydration: maintaining consistent eating patterns helps stabilize digestion
IBS pain may vary from day to day, but understanding where it originates – and how to regulate your gut–brain communication – can help you take back control.
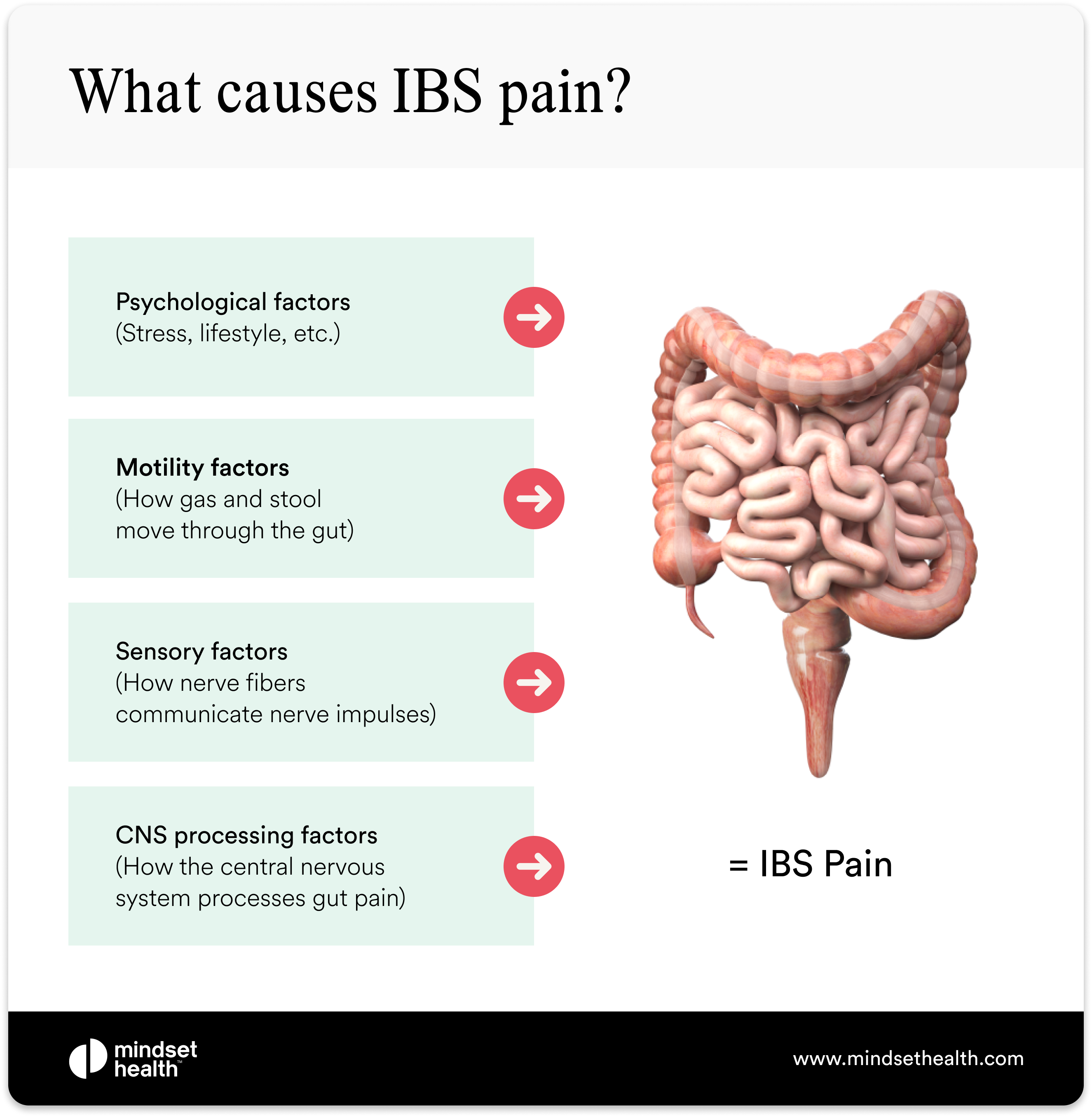
What causes IBS pain?
You can think about IBS pain in two ways. First, pain may be caused or worsened by the physical and social factors associated with IBS (such as stress or how gas moves through the bowels). Second, pain may be caused by how IBS affects the pain-signaling function of the nervous system between the brain and the gut. Abdominal IBS pain is typically referred to as a type of visceral pain. Unlike somatic pain, which is felt by the skin, muscles, bone, and soft tissues, visceral pain is felt around the internal organs, including the stomach and intestines.
People with IBS need to understand that while pain is felt in different areas of the body, it is processed in the brain.
Why IBS pain happens: the gut-brain connection explained
Research into IBS suggests that pain often stems from oversensitive nerves in the gut. These nerves send stronger-than-normal signals to the brain, causing it to interpret regular digestive sensations as painful or threatening.
Millions of nerves and neurons run between the gut and brain along a neural pathway known as the gut-brain axis. This system allows two-way communication – the brain can sense what’s happening in the gut, and the gut can sense what’s happening in the brain. That’s why you might feel “butterflies” in your stomach before a big event or lose your appetite when you’re anxious.
The brain doesn’t just receive pain messages; it can also shape how those messages are processed. When hypersensitive gut nerves send mixed or amplified signals, the brain may overestimate or misinterpret the information it receives – registering more pain than what’s physically occurring. This mechanism, known as the gate control theory of pain, helps explain why people with IBS often experience heightened or prolonged discomfort even without visible inflammation or injury.
Understanding this gut-brain signaling helps explain why stress management, vagus nerve activation, and relaxation techniques can all help reduce IBS pain over time.
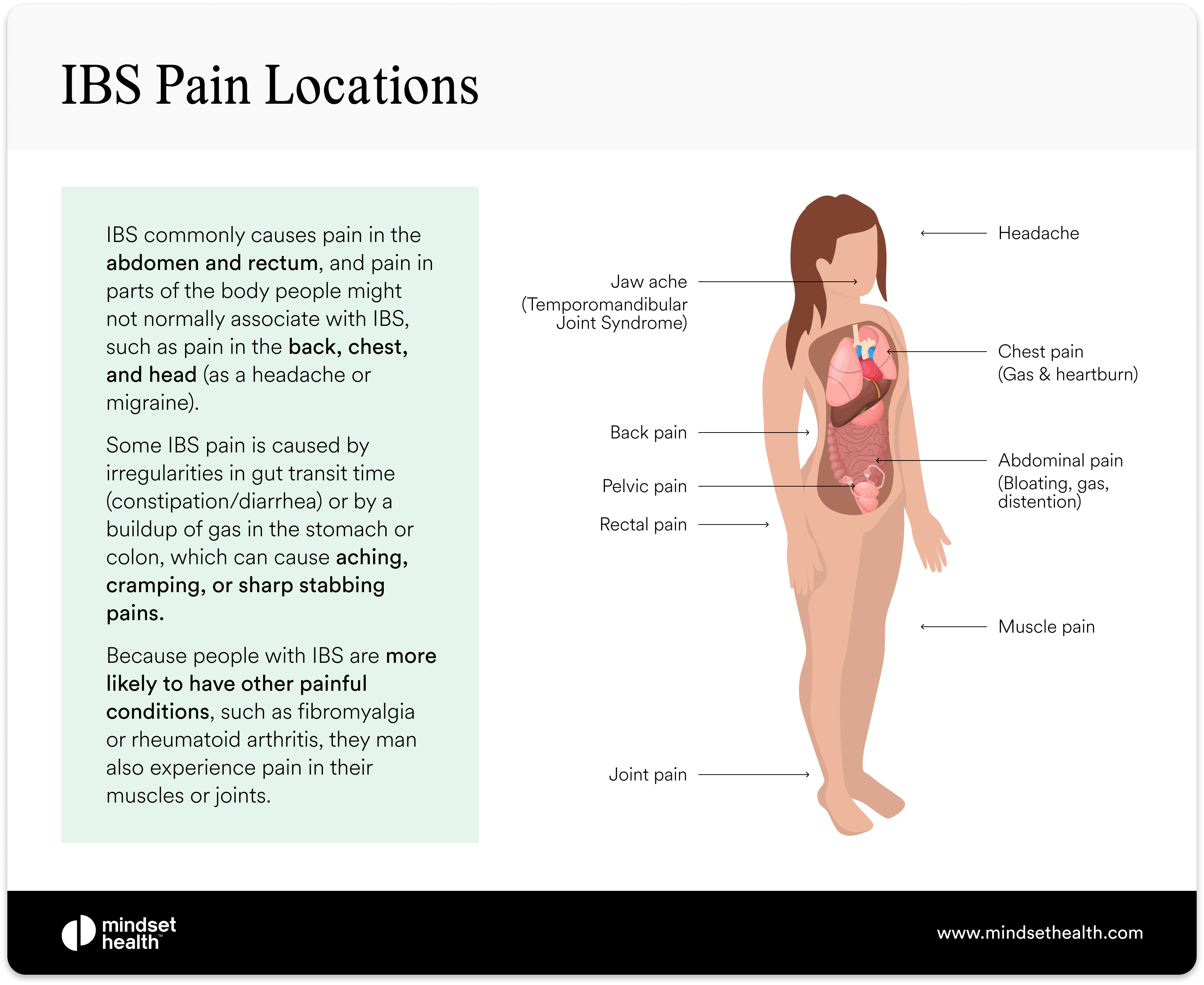
IBS pain locations
While gut pain is a common IBS symptom, pain unrelated to the digestive tract is also common in people with IBS.
IBS abdominal pain: causes, triggers, and what it feels like
Abdominal pain is one of the most frequently reported IBS symptoms and often occurs alongside nausea, tenderness, and bloating. The pain typically develops from trapped gas or muscle contractions in the intestines, which can lead to disordered defecation – meaning constipation, diarrhea, or both.
This discomfort is often centered around the navel but can also appear on the left or right side of the abdomen. Because IBS pain can move or shift location, it’s not always easy to pinpoint one specific area. The intensity may vary from a dull ache to sharp cramping that flares after meals or during stressful moments.
Psychological factors such as stress and anxiety also play a major role in abdominal pain. When the sympathetic nervous system activates the body’s fight-or-flight response, blood flow is redirected away from the digestive tract, slowing gut function. This can lead to constipation, bloating, and additional pain.
For many people, IBS abdominal pain tends to worsen after eating, during times of high stress, or around hormonal changes such as a woman’s menstrual cycle. Understanding these triggers – and how the gut-brain connection responds to them – is key to reducing pain episodes and improving overall digestive comfort.
IBS gas pain: causes, sensitivity, and relief options
A buildup of gas in the intestines can be one of the most painful and frustrating IBS symptoms. Gas pain is typically felt across the abdomen and can range from mild cramping to sharp, stabbing sensations that mimic more serious conditions.
For most people with IBS, the pain isn’t caused by producing more gas than average – it’s caused by increased gut sensitivity to normal amounts of gas. This means your digestive nerves overreact to stretching or distention in the intestines, amplifying discomfort and bloating.
Gas enters the gastrointestinal tract in two main ways:
- Swallowing air (aerophagia) – air taken in while eating, drinking, chewing gum, or smoking.
- Bacterial fermentation – gut bacteria breaking down undigested food and releasing gas as a byproduct.
Normally, gas leaves the body through burping or flatulence. But in IBS, gas can become trapped, leading to abdominal pressure, visible bloating, and pain.
A 2011 study highlighted three main reasons people with IBS may experience more gas pain and bloating than those without gut problems:
- Difficulty moving gas through the intestines – some people have slower or disordered gut motility, which can cause gas to build up and stretch the intestinal walls.
- Difficulty evacuating gas – people with IBS, constipation, or functional bloating may be less able to pass gas effectively, increasing distention and discomfort.
- Increased gut sensitivity – IBS patients are more sensitive to normal stretching of the gut, meaning even small amounts of gas can cause significant pain.
Therapies that help regulate gut-brain communication, such as gut-directed hypnotherapy, have been shown to lower visceral hypersensitivity and reduce gas pain without relying on medication or restrictive diets. Programs like Nerva make this approach more accessible, allowing people to retrain their gut’s pain response and relieve symptoms from home.
Do men and women experience IBS gas pain differently?
Yes – while both men and women with IBS can experience gas pain, bloating, and abdominal discomfort, the pattern and severity of symptoms can differ due to hormonal, anatomical, and physiological factors.
Women with IBS
Women often report gas pain in the abdomen, lower back, and pelvic region. This discomfort is linked to heightened intestinal sensitivity and abnormal gut contractions, which can intensify during hormonal fluctuations across the menstrual cycle. Estrogen and progesterone changes can influence how the gut muscles move and how sensitive the intestines feel, leading to more bloating and cramping.
Because of these overlapping symptoms, endometriosis is sometimes mistaken for IBS. Both conditions can cause pelvic pain, bloating, and changes in bowel habits, but endometriosis requires different diagnostic methods and treatment approaches. Recognizing the distinction between the two is crucial for proper management.
Men with IBS
Men may experience gas pain in similar areas – the abdomen, lower back, and pelvic region – but hormonal influences tend to play a smaller role. Instead, men often describe their discomfort as pressure, tightness, or cramping caused by increased intestinal sensitivity and irregular muscle contractions in the gut.
Understanding how gender differences, hormones, and gut sensitivity interact can help tailor IBS management strategies more effectively, improving comfort and reducing the likelihood of misdiagnosis.

Calm your IBS in 6 weeks
Take our free assessment to discover if Nerva can work for you.
✅ 89% success rate
✅ 80,000+ people helped
✅ Created by gut health experts
❌ No appointments or waitlists
❌ No pills or diet change
Start assessmentHot Flash Relief
Manage your hot flashes in just 5 weeks.
✅ Science-backed & effective
✅ Natural & safe option
✅ Created by Dr Elkins
❌ No appointments or waitlists
❌ No medications
Learn moreRefer, monitor and grow
A free and easy way to refer patients to digital hypnotherapy programs.
Let's Connect.webp)
.webp)
IBS back pain: why it happens and how it’s connected
Back pain isn’t a symptom most people associate with IBS – but it’s surprisingly common. Research shows that between 68% and 81% of people with IBS experience some form of back pain, often linked to gas buildup, bloating, or colonic spasms.
In many cases, back pain in IBS is what’s known as referred pain – discomfort that originates in one area of the body (such as the intestines) but is felt elsewhere. This happens because the nerves that carry pain signals from the gut overlap with those that serve the lower back. Just as heart pain can radiate to the jaw or menstrual cramps can trigger backache, intestinal pain from IBS can be felt along the spine or lower back.
Back pain in IBS can also occur because people with IBS are more likely to have overlapping conditions that affect muscles, joints, or connective tissue, such as fibromyalgia, rheumatoid arthritis, or interstitial cystitis (a chronic bladder pain condition). These conditions share similar pain pathways and nervous system sensitivities.
According to the UNC Center for Functional GI & Motility Disorders, up to 60% of people with IBS also experience fibromyalgia, and around 70% of those with fibromyalgia experience IBS symptoms. This overlap highlights how widespread nervous system hypersensitivity can amplify pain signals throughout the body – not just in the gut.
Understanding that IBS-related back pain often stems from nerve cross-communication and shared pain pathways can help guide more effective management strategies, including movement, gentle stretching, and therapies that target both muscle tension and the gut-brain connection.
IBS chest pain: understanding the link between gas, reflux, and nerve sensitivity

Chest pain can sometimes indicate a serious heart condition, such as coronary artery disease, but for many people with IBS, it’s often linked to trapped gas or acid reflux rather than cardiac problems.
While gas pain is more commonly felt in the lower abdomen, it can also move upward when gas becomes trapped in the stomach or left portion of the colon, both of which sit close to the chest. This pressure can cause sharp, tight, or stabbing sensations that may feel alarmingly similar to heart pain.
People with IBS are also four times more likely to experience gastroesophageal reflux disease (GERD) – also known as chronic acid reflux or heartburn. GERD causes burning or squeezing pain behind the breastbone, especially after eating or when lying down, and can easily be mistaken for heart pain.
Dr. Rao Satish, Director of Neurogastroenterology and GI Motility at the University of Iowa, explains:
“The nerves that supply the heart also supply the esophagus. Therefore, patients may think they are experiencing pain of a cardiac origin when the pain is, in fact, coming from the esophagus.”
Researchers believe the overlap between GERD and IBS may be linked to poor muscle function throughout the digestive tract. A study published in the World Journal of Gastroenterology, by Dr. Nicola de Bortoli found that motor abnormalities – disruptions in how the muscles of the esophagus, stomach, and intestines contract – could explain why the two conditions often occur together.
If you experience chest pain, it’s always important to rule out heart disease first. Once serious causes are excluded, addressing gut motility, reflux management, and gas relief through lifestyle adjustments, stress regulation, and medical guidance can help ease discomfort and restore digestive balance.
IBS headache and migraine pain: understanding the gut-brain connection
How can an irritable gut make your head irritable too? Head and gut pain may seem unrelated, but research shows a strong connection between IBS, headaches, and migraines.
A study published in the Polish Journal of Neurology and Neurosurgery found that between 23% and 53% of people with IBS experience frequent headaches. Similarly, research in the Journal of BMC Gastroenterology reported that people with IBS are about 60% more likely to experience migraines than those without the condition.
This overlap is explained by the gut-brain axis – the bidirectional communication system linking the nervous system of the gut and the brain. When the gut is inflamed, stressed, or hypersensitive, it can influence neurotransmitters and pain pathways that affect the brain, increasing the likelihood of headaches and migraine flare-ups.
The relationship works both ways. Just as people with IBS commonly experience headaches, many migraine sufferers also develop digestive symptoms such as nausea, vomiting, abdominal pain, or diarrhea during migraine attacks. This shared pathway suggests that both IBS and migraines may arise from similar dysfunctions in nerve signaling, stress response, and serotonin regulation.
Understanding how gut and brain sensitivity interact helps explain why therapies that calm the nervous system – such as gut-directed hypnotherapy, relaxation breathing, and stress reduction – can often ease both digestive pain and headache frequency.
How IBS and headaches are connected
While the exact reason for the overlap between IBS and headaches isn’t fully understood, research points to the shared communication network between the gastrointestinal system and the central nervous system – known as the gut-brain axis.
The vagus nerve, the body’s longest cranial nerve, plays a central role in this connection. It carries signals in both directions between the gut and the brain, meaning it can relay pain messages, stress responses, and sensory information back and forth. Because the vagus nerve influences both migraine activity and IBS symptoms, it’s often thought to be a key factor in why these two conditions commonly occur together.
Research also identified two neuropeptides– chemical messengers that communicate along the gut-brain axis – which may contribute to both migraine pain and gastrointestinal sensitivity. These shared biochemical pathways help explain why people with IBS are more likely to experience migraines, and why those with migraines often report gut-related symptoms such as nausea or abdominal discomfort.
The good news is that the gut-brain connection works in both directions. While stress or gut dysfunction can trigger headaches, calming the mind and regulating the nervous system can also improve gut health. This is why therapies such as gut-directed hypnotherapy have been shown to relieve both digestive and headache symptoms without relying on medication or restrictive diets, helping to restore balance across the entire gut-brain network.
IBS jaw and face pain
IBS can be such a pain in the...face? The research suggests that people with IBS are at a greater risk of experiencing joint and face pain due to a higher likelihood of experiencing other centralized chronic pain conditions.
One recent study showed that people with any subtype of IBS were three times more likely to experience pain and compromised movement of the jaw joint and the surrounding muscles due to Temporomandibular disorders (TMDs).
According to John Hopkins Medicine, TMDs are disorders of the jaw muscles, temporomandibular joints (the sliding hinges connecting your jaw to your skull), and the nerves associated with chronic facial pain.
Similar to IBS, current research suggests that hypnosis may also be an effective tool for treating TMD pain.
IBS anal and rectal pain: what causes it and when to see a doctor
IBS – particularly IBS-C (constipation-predominant IBS) – can lead to secondary complications such as hemorrhoids and anal fissures, both of which cause anal and rectal pain or bleeding. Because constipation often results in hard, dry, and difficult-to-pass stools, this pain is usually most noticeable during or immediately after a bowel movement.
External hemorrhoids (often called “piles”) are swollen veins in the anus or rectum, similar to varicose veins. They can become irritated, inflamed, or even tear slightly, leading to sharp pain or soreness. Prolonged straining, sitting on the toilet, or frequent bowel movements can all worsen hemorrhoids – which is why they’re commonly associated with IBS symptoms such as constipation or diarrhea.
Research also shows that people with hemorrhoids often report other IBS-like symptoms, including bloating, abdominal discomfort, and reduced quality of life, suggesting a strong association between the two conditions.
An anal fissure is a small tear in the lining of the anus, usually caused by passing a hard stool during constipation or frequent, loose stools from diarrhea. These fissures can lead to burning pain, bleeding, and irritation that lingers after defecation.
A 2017 study screening 255 people with irritable bowel syndrome.found that 27.8% also had a history of anal complications such as fissures, reinforcing how bowel irregularity can contribute to anal pain.
While mild bleeding or soreness may be a temporary side effect of IBS, any persistent pain, large amounts of blood, or black, tarry stools should be assessed by a doctor immediately. These symptoms can sometimes indicate more serious conditions, including bowel cancer or other gastrointestinal disorders.
Maintaining soft, regular bowel movements through hydration, dietary fiber, and stress management can help prevent hemorrhoids and fissures, while treatments such as topical ointments, warm baths, and medical evaluation can relieve pain and promote healing.
Best pain medications for IBS: what works and what to avoid
If you’re used to reaching for a pill to manage IBS pain, it may be time to reconsider your approach. Many common over-the-counter pain relievers provide only temporary relief — and some can actually worsen gut symptoms over time.
Non-steroidal anti-inflammatory drugs (NSAIDs) such as Advil, Motrin, and Aleve, along with acetaminophen (Tylenol, Paracetamol, Panadol) and aspirin, are often used to relieve abdominal pain because of their anti-inflammatory and pain-reducing effects. However, research published in the Journal of Anesthesiology and Pain Medicine found limited evidence supporting the effectiveness of these medications for IBS pain and noted that long-term use can contribute to chronic constipation — a problem for anyone already struggling with bowel irregularity.
Frequent use of NSAIDs also appears to have negative effects on people with IBS. Studies show a potential link between regular NSAID use and the development or worsening of IBS symptoms, likely due to the drugs’ impact on the intestinal lining and gut microbiota.
If you want to try an over-the-counter pain reliever, acetaminophen may be a safer choice. It’s gentler on the stomach and doesn’t carry the same risk of intestinal irritation or constipation. In contrast, pain-relieving NSAIDs like ibuprofen and naproxen are known to cause gastrointestinal issues — from mild indigestion and reflux to more serious problems such as ulcers when used long term.
For lasting relief, addressing the root causes of IBS pain through gut-brain therapies, stress regulation, and dietary strategies is more effective than relying on standard painkillers. A healthcare provider can also guide you toward safer, evidence-based options tailored to your type of IBS and symptom pattern.
Common IBS pain treatments: effective ways to find relief
There are many ways to manage IBS pain without relying on NSAID pain medications. Because IBS pain stems from both physical factors and miscommunication between the gut and brain, treatment often involves a mix of lifestyle, dietary, and relaxation-based approaches.
Abdominal pain
Because IBS abdominal pain is caused by physical factors and miscommunicating pain signals in the gut and the brain, there are several helpful things you can do to ease symptoms.
For abdominal pain, try taking peppermint oil, taking antispasmodics (like Buscopan), applying a heat pack, or trying gut-directed hypnotherapy.
Gas pain
To reduce gas pain, you can try an over-the-counter treatment like Simethicone, which is available as Gas-X, Mylanta Gas, or Phazyme, though there is little objective evidence of its benefit over placebo. Similarly, a small study of five volunteers taking activated charcoal for gas made no difference in levels of gas production nor abdominal symptoms.
If you can manage the pain, exercises like very gentle crunches and some yoga positions are known to help dislodge acute gas trapped in the colon.
The best treatment for gas is often prevention. Expert advice for reducing gas and bloating includes restricting wheat-fiber, limiting fat intake, and avoiding carbonated drinks, and artificial sweeteners.
Back pain
As back pain from IBS is often caused by gas, it's a good idea to try and avoid foods and drinks that increase gas production. A 2006 study in The American Journal of Gastroenterology found exercise can help trapped gas move through your digestive system, and relieve gas and bloating.
While laying down might seem like a good remedy for back pain, research has shown that gas retention can actually sometimes worsen symptoms when you're laying down. To reduce backache, try to do some light exercise and minimize periods of reclining rest during the day.
Chest pain
If you're experiencing chest pain due to a combination of IBS and acid reflux, taking antacids, such as Mylanta, Rolaids, and Tums, may help soothe burning pain. Make sure you talk to your doctor about chest pain, as it may be a sign of another condition.
Headaches/jaw pain/face pain
Unlike abdominal IBS pain, which is usually unlocalized and visceral pain, headache and jaw and face pain are somatic, which means it's localized to the pain receptors in one specific area.
Two common treatments for somatic pain are non-steroidal anti-inflammatory drugs (NSAIDs) and acetaminophen (Tylenol, Paracetamol) — but remember that if you take an NSAID (like Advil, Motrin, or Aleve), you might end up fixing your headache but make your gut symptoms worse.
Anal/rectal pain
Sitz baths (shallow baths with warm water), several times a day for 10-20 minutes at a time, may help relieve pain and swelling associated with hemorrhoids or anal fissures.
Stool softeners may help to relieve symptoms and the pain of defecating; however, laxatives can lead to additional irritation. For pain, itching, or swelling, over-the-counter topical creams, ointments, or cortisone suppositories may help. Avoid hemorrhoid treatments promising to numb pain (medications ending in “-caine”) as they can cause irritation with long-term use.
When to see a doctor about IBS pain
If you’re dealing with ongoing or severe IBS pain, it’s a good idea to book an appointment with a healthcare professional. A doctor can confirm your diagnosis, assess whether your symptoms match IBS, and rule out other gastrointestinal conditions that may need different treatment.
While IBS pain is common, certain symptoms may signal a more serious digestive issue. See your doctor right away if you experience any of these IBS red flags:
- Rectal bleeding or blood in your stool
- Unexplained weight loss
- A family history of bowel or colon cancer
- Ongoing fever or signs of infection
- IBS symptoms appearing or worsening after age 50
These symptoms don’t always mean something serious is wrong – but they do require medical evaluation to rule out conditions such as inflammatory bowel disease, bowel cancer, or infection. Early diagnosis and appropriate care can help you manage symptoms safely and effectively.
FAQs about IBS pain
Where is IBS pain usually felt?
IBS pain is most often felt in the lower abdomen, but it can also appear in other areas such as the back, chest, head, jaw, face, or rectum. The pain may shift locations and vary in intensity, from dull aching to sharp cramps.
Why does IBS cause pain?
Pain occurs when the nerves in the gut become oversensitive, sending amplified pain signals to the brain. This miscommunication along the gut-brain axis can make normal digestive sensations feel painful or uncomfortable.
What does IBS pain feel like?
IBS pain can feel like cramping, bloating, pressure, or sharp stabbing sensations. It may worsen after eating, during stress, or around hormonal changes such as menstruation.
Can IBS cause pain outside the abdomen?
Yes. Because IBS involves the gut-brain axis and overall nervous system sensitivity, pain can also appear in other areas like the back, chest, or jaw. These are often examples of referred pain – when pain is felt in a different location from where it originates.
Which pain medications are safe for IBS?
Acetaminophen (Tylenol, Paracetamol) is generally considered safer for IBS pain. NSAIDs such as Advil, Motrin, or Aleve should be avoided, as long-term use can irritate the gut and increase the risk of ulcers or constipation.
What are the best natural remedies for IBS pain?
Many people find relief with at-home strategies such as peppermint oil, antispasmodic medications like Buscopan, applying a heat pack, gut-directed hypnotherapy, diaphragmatic breathing, and stress reduction techniques.
When should I see a doctor about IBS pain?
Consult a doctor if you experience severe or persistent pain, or if you notice red flag symptoms such as rectal bleeding, unexplained weight loss, fever, a family history of colon cancer, or new symptoms appearing after age 50.
The wrap up
IBS can cause pain across many parts of the body – most commonly in the abdomen, but also in areas such as the back, chest, head, jaw, and rectum. While many people turn to over-the-counter options for relief, medications like NSAIDs (Advil, Motrin, Aleve) are not proven to help IBS pain and may irritate the stomach or intestines over time.
At-home remedies such as peppermint oil, antispasmodics like Buscopan, heat packs, and gut-directed hypnotherapy can be effective for easing discomfort and regulating the gut-brain connection. If your pain is persistent or severe, it’s important to speak with your doctor to confirm your diagnosis, rule out other conditions, and develop a safe, evidence-based plan for long-term symptom relief.
Want to calm your IBS in 15 minutes a day?
Take our free quiz to discover if Nerva's gut-directed hypnotherapy program can work for you.
✅ 89% success rate
✅ 80,000+ people helped
✅ Created by gut health experts
❌ No appointments or waitlists
❌ No pills or diet change
Start quizHot Flash Relief
Manage your hot flashes in just 5 weeks.
✅ Science-backed & effective
✅ Natural & safe option
✅ Created by Dr Elkins
❌ No appointments or waitlists
❌ No medications
Learn moreRefer, monitor and grow
A free and easy way to refer patients to digital hypnotherapy programs.
Let's ConnectTake the Quiz.
Take the Quiz.


.svg)

.png)







